Eosinophilic asthma is a subtype of asthma characterized by a higher than normal presence of eosinophils, a type of white blood cell, in the lungs and blood. Eosinophils play a critical role in the immune system, often increasing in number to fight off certain infections and diseases.
However, in eosinophilic asthma, these cells contribute to inflammation and swelling in the airways, leading to the chronic symptoms associated with this condition.
Patients with eosinophilic asthma typically experience common asthma symptoms, including shortness of breath, chest tightness, wheezing, and coughing. These symptoms result from the narrowing of the airways due to inflammation. However, this specific type of asthma is often more severe and less responsive to standard treatments compared to other forms of asthma, making it important to identify and manage properly.
Eosinophilic Asthma Symptoms & Signs

Eosinophilic asthma is characterized by specific respiratory symptoms and is often associated with particular comorbid conditions. Patients generally experience severe asthma symptoms that may not respond well to standard treatments.
Respiratory Symptoms
Individuals with eosinophilic asthma typically suffer from severe asthma attacks that are distinguished by heightened respiratory symptoms. These symptoms include:
- Chest tightness: Patients often describe a sensation of tightness in the chest, which can indicate airway constriction.
- Shortness of breath: Difficulty in breathing, or dyspnea, is common and can occur both during physical activity and at rest.
- Wheezing: A high-pitched whistling sound while breathing is a hallmark of airway obstruction.
- Coughing: Persistent cough that is often dry and unproductive, exacerbating breathing difficulties.
Associated Conditions
The following conditions are frequently associated with eosinophilic asthma and can impact its management:
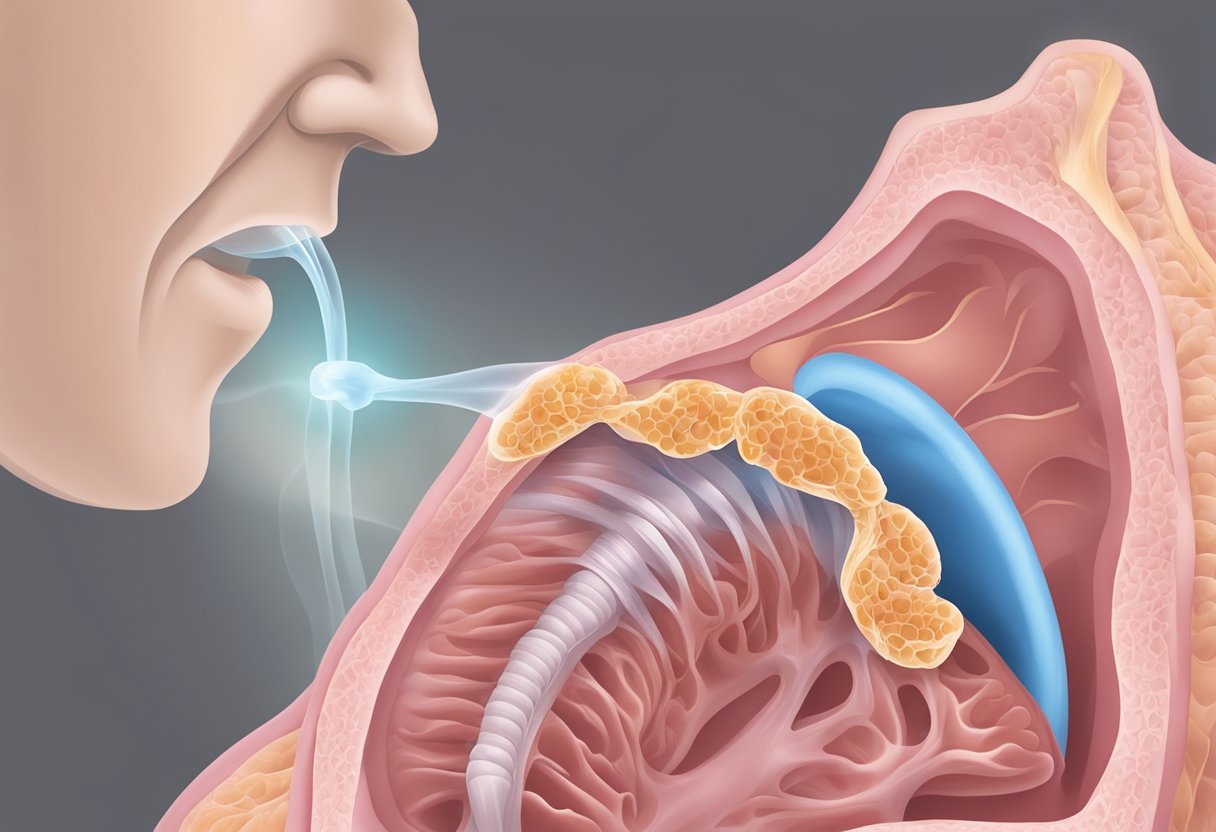
- Nasal polyps: Soft, noncancerous growths that can form in the sinuses or nasal passages, potentially leading to chronic sinus blockages.
- Chronic sinusitis: Also known as rhinosinusitis, this condition involves prolonged inflammation of the sinuses, often with nasal polyps, contributing to respiratory challenges.
Diagnosis
Diagnosing eosinophilic asthma involves a series of examinations to identify the specific characteristics distinguishing it from other forms of asthma.
Physical Examination
During the physical examination, the doctor assesses the patient for signs of respiratory distress and listens to their lungs for any wheezing indicative of obstruction. They may also inspect the nasal passages for signs of inflammation or polyps, which are often associated with asthma.
Diagnostic Tests
Diagnostic tests play a crucial role in confirming eosinophilic asthma. The following table and list detail the primary tests utilized:
| Test Type | Purpose |
|---|---|
| Blood Test | To measure eosinophil levels and rule out infections |
| Lung Function Test | To evaluate the extent of airway obstruction |
| Sputum Analysis | To detect eosinophils in the mucus |
| Bronchial Biopsy | To examine tissue for signs of eosinophils and inflammation |
| Allergy Tests | To identify potential allergens triggering asthma |
Blood Tests: These are used to count eosinophil levels. Elevated eosinophil counts can indicate the presence of eosinophilic asthma, but they may also suggest parasitic infections which must be ruled out.
Lung Function Tests: These tests, including spirometry, measure how well the lungs are working and the degree of any obstruction.
Sputum Analysis: Doctors may collect sputum to analyze under a microscope for the presence of eosinophils.
Bronchial Biopsy: In some cases, a biopsy of the bronchial airways may be conducted to check for eosinophilic inflammation.
Allergy Tests: Skin or blood tests determine if specific allergens contribute to asthma symptoms.
Understanding Eosinophilic Asthma
Eosinophilic asthma is a complex condition affecting the respiratory system, primarily characterized by elevated levels of eosinophils—an integral part of the immune system. This chronic subtype of asthma predominantly affects adults and involves persistent lung inflammation.
Definition and Overview
Eosinophilic asthma is a specific subtype of asthma where lung inflammation is associated with a high number of eosinophils in the lung tissue and blood. Eosinophils are a type of white blood cells that are a normal component of the immune system but can contribute to inflammation and tissue damage when present in excess. This form of asthma typically occurs in adults, reflecting a chronic, long-term respiratory condition that often requires specialized management.
Causes and Triggers
The exact causes of eosinophilic asthma are not completely understood, but certain allergens and environmental factors can serve as triggers. These triggers may include:
- Indoor allergens such as dust mites, pet dander, and molds
- Outdoor allergens like pollen and air pollution
- Respiratory infections
- Occupational irritants
These triggers can prompt the immune system to release eosinophils into the bloodstream and the lung tissue, exacerbating respiratory symptoms and inflammation.
Eosinophils and Inflammation
In eosinophilic asthma, lung inflammation is a key factor in the chronic symptoms experienced by patients. Eosinophils release substances that can damage lung tissues and exacerbate asthma symptoms. Due to the persistent nature of this inflammation, it can lead to:
- Difficulty breathing
- Frequent asthma exacerbations
- Reduced lung function
Monitoring and controlling the level of eosinophils in the blood are vital in managing the condition to reduce the risk of severe asthma attacks and improve overall respiratory health.
Eosinophilic Asthma Treatment and Management
Eosinophilic asthma is a complex condition requiring a tailored approach to treatment. The management typically focuses on reducing inflammation, preventing symptoms, and minimizing flare-ups using a combination of medications and biologic therapies.
Medications
The cornerstone of eosinophilic asthma treatment involves the use of medications to control inflammation and alleviate symptoms. The following are key pharmaceutical treatments:
- Inhaled Corticosteroids (ICS): Used daily to reduce airway inflammation and prevent asthma attacks.
- Corticosteroids: Systemic corticosteroids may be prescribed for short-term use during severe flare-ups.
Patients need to adhere to their treatment plan, which often includes taking these medications regularly and monitoring their condition closely.
Biologic Therapies
Biologic therapies represent a significant advancement in the treatment of eosinophilic asthma, targeting specific cells and pathways involved in the inflammatory process. Here are some biologic drugs used in the management of this condition:
- Omalizumab (Xolair): Targets and blocks IgE antibodies.
- Mepolizumab (Nucala): A monoclonal antibody that blocks interleukin-5 (IL-5).
- Reslizumab (Cinqair): Also targets IL-5, reducing eosinophil count.
- Benralizumab (Fasenra): Binds to the IL-5 receptor on eosinophils and basophils.
- Dupilumab (Dupixent): Inhibits the signaling of IL-4 and IL-13, two key drivers of inflammation.
Biologic treatments are generally administered through injections or infusions under the guidance of a healthcare professional, and can greatly improve quality of life for those with severe eosinophilic asthma.
Living with Eosinophilic Asthma
Living with eosinophilic asthma involves ongoing management and adjustment of lifestyle to maintain a high quality of life. The following sections detail specific strategies for managing daily activities and coping with the condition.
Lifestyle Adjustments
Individuals with eosinophilic asthma may find that their condition necessitates changes to daily routines to minimize the risk of flare-ups and maintain overall health. Key adjustments include:
- Avoiding Allergens and Irritants: Steering clear of smoke, dust, and other potential allergens can help prevent exacerbation of symptoms.
- Rest: Ensuring adequate rest is critical, as fatigue can worsen asthma symptoms.
- Exercise: Moderate exercise should be encouraged, but it’s essential to consult with a healthcare provider to tailor physical activities appropriately.
Coping Strategies
Developing coping mechanisms can significantly enhance an individual’s ability to manage eosinophilic asthma and its impact on their life. Strategies include:
- Asthma Education: Understanding the condition can empower patients to make informed decisions about their healthcare and daily activities.
- Stress Management: Reducing stress through techniques such as mindfulness or yoga can decrease the likelihood of severe asthma attacks.
- Regular Medication Use: Adherence to prescribed asthma drugs is vital to control inflammation and prevent symptoms.
This article is for informational purposes only. If you believe you or a loved one may be showing signs of this health condition, please seek immediate medical attention for appropriate diagnosis and treatment.






